Systemic Bias in Health Algorithms
Health Disparities and Importance of Zip Codes
Read the latest on Health from Heart and Soul Magazine..and NMQF
NMQF Sickle Cell Disease Working Group to Introduce New Data Mapping Platform
NMQF will introduce the SCD Index at the SCDAA National Convention, Friday Oct 11th at 4:15 p.m. The index is the first of its kind to map aggregated SCD data in the US by population statistics as well as health cost and utilization. The index is searchable by demographics and geographies with other capabilities to be shared. We welcome those interested in advancing knowledge and quality of care. To learn more contact us at index@nmqf.org
Quite a Picture !…Disparities in Clinical Trials…Why Not More Noise About This?
NMQF Sickle Cell Disease working group to present at the SCDAA Annual Meeting in Baltimore on Oct 11, 4:15 p.m. The presentation will introduce the first SCD Index mapping U.S. population statistics, as well as health cost and utilization related to SCD….searchable by demographics and geographies.
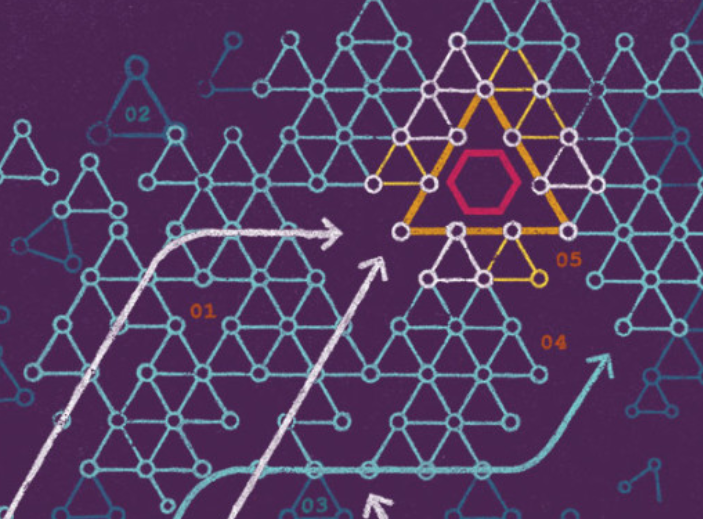
At the recent AACR meeting in San Francisco NMQF Cancer Working Group members and stakeholders presented an interesting poster about the location of clinical trials and prevalence of lung cancer among minorities. The visual says a lot. lungcancerposteraacrSEPT 2019
Index partners build knowledge and solutions to improve clinical trials: https://cancerres.aacrjournals.org/content/79/13_Supplement/LB-012
Identifying Racial and Ethnic Disparities in Human Services

Urban.org: Marla McDaniel, Tyler Woods, Eleanor Pratt, Margaret Simms
Abstract
Introduction
When there is evidence of racial and ethnic differences at any point in the service delivery spectrum—for example, in access to and take-up of human services, in the nature and quality of services received, or in the outcomes of services—it can be challenging to interpret what those differences mean. In particular, it can be challenging to understand whether and to what extent those differences represent disparities. Disparities mean that one group is systematically faring worse than another for reasons that are not due to the group’s needs, eligibility, or preferences.
This report helps the Administration for Children and Families (ACF) build the base of knowledge necessary to reliably identify and interpret racial and ethnic differences in relation to ACF’s human services programs. Better understanding these differences and being able to distinguish when those differences indicate disparities can help improve ACF’s program delivery. To further ACF’s understanding, this report synthesizes the existing research on racial and ethnic differences and disparities in relation to the service delivery systems of six programs, or program areas, administered by ACF:
- Temporary Assistance for Needy Families (TANF)
- Child Support Enforcement Program
- Child Care and Development Fund
- Head Start
- Family and Youth Services Bureau programs for runaway and homeless youth and adolescent pregnancy prevention
To facilitate this synthesis, the report provides a clear definition of disparities. It also develops a conceptual framework for identifying racial and ethnic differences throughout the service delivery system and for distinguishing racial and ethnic differences from disparities. READ FULL ARTICLE
Eliminating Racial/Ethnic Disparities in Health Care: What are the Options?

Kaiser Family Foundation
Racial and ethnic disparities in health care – whether in insurance coverage, access, or quality of care – are one of many factors producing inequalities in health status in the United States.1 Eliminating these disparities is politically sensitive and challenging in part because their causes are intertwined with a contentious history of race relations in America. Nonetheless, assuring greater equity and accountability of the health care system is important to a growing constituency base, including health plan purchasers, payers, and providers of care. To the extent that inequities in the health care system result in lost productivity or use of services at a later stage of illness, there are health and social costs that affect us all.
Why Health Care Disparities Are a Concern
One in three residents of the United States self-identify as either African American, American Indian/Alaska Native, Asian, Native Hawaiian/Pacific Islander, Hispanic/Latino, or multiracial. By 2050, this number is expected to increase to one in two.2
Despite significant advances in civil rights, race remains a significant factor in determining whether an individual receives care, whether an individual receives high-quality care, and in determining health outcomes.
The Institute of Medicine (IOM) landmark report, Unequal Treatment, provides compelling evidence that racial/ethnic disparities persist in medical care for a number of health conditions and services.3 Numerous efforts are underway to reduce or eliminate racial and ethnic health care disparities, and to address some of the social factors that affect health care outcomes. Yet despite these many efforts, disparities in access to quality care remain, and for some measures being tracked, gaps in care are getting larger rather than smaller.4
Key Facts on Race, Ethnicity and Health Care in the U.S.
- Racial/ethnic disparities in health persist today even when comparing groups of similar SES. For example, the infant mortality rate for college-educated Black women is higher than that for White women with similar education (11.5 vs. 4.2 per 1,000 live births).
- The rate of new AIDS cases in 2003 was 3 times higher among Hispanics and 10 times higher among African Americans than among Whites (26 and 75 per 100,000 vs. 7 per 100,000).
- At least 1 in 3 nonelderly Latinos (36%) and AI/ANs (33%) is uninsured, as compared with 22% of African Americans, 17% of Asian and Pacific Islanders, and 13% of Whites.
- Insurance matters, as evidence by the fact that uninsured adults across racial/ethnic groups are at least twice as likely to go without a doctor visit in the past year.
- Black and Latino adults are less likely to rely on a private physician for their medical care than White adults (62% and 44% vs. 77%).
- African American children have a rate of hospitalization for asthma that is 4 to 5 times higher than the rate for White children (527 per 100,000 vs. 144 per 100,000).
- Disparities in quality of care are not getting smaller. Over time, the gap between Whites and African Americans, Hispanics, Asians, and AI/ANs has either remained the same or worsened for more than half of the core quality measures being tracked.
ADDRESSING HEALTH CARE DISPARITIES
Although attention to racial/ethnic disparities in care has increased among policymakers, there is little consensus on what can or should be done to reduce these disparities. The U.S. Congress provided early leadership on the issue by legislatively mandating the IOM study on health care disparities, creating the National Center on Minority Health and Health Disparities at the National Institutes of Health, and requiring DHHS to produce the National Healthcare Disparities Report.5 This brief examines four broad policy areas for addressing racial and ethnic health care disparities: READ FULL ARTICLE
Reducing Racial and Ethnic Disparities in Access to Care: Has the Affordable Care Act Made a Difference?
Abstract
- Issue: Prior to the Affordable Care Act (ACA), blacks and Hispanics were more likely than whites to face barriers in access to health care.
- Goal: Assess the effect of the ACA’s major coverage expansions on disparities in access to care among adults.
- Methods: Analysis of nationally representative data from the American Community Survey and the Behavioral Risk Factor Surveillance System.
- Findings and Conclusions: Between 2013 and 2015, disparities with whites narrowed for blacks and Hispanics on three key access indicators: the percentage of uninsured working-age adults, the percentage who skipped care because of costs, and the percentage who lacked a usual care provider. Disparities were narrower, and the average rate on each of the three indicators for whites, blacks, and Hispanics was lower in both 2013 and 2015 in states that expanded Medicaid under the ACA than in states that did not expand. Among Hispanics, disparities tended to narrow more between 2013 and 2015 in expansion states than nonexpansion states. The ACA’s coverage expansions were associated with increased access to care and reduced racial and ethnic disparities in access to care, with generally greater improvements in Medicaid expansion states.
Background
Historically, in the United States, there has been a wide gulf between whites and members of minority groups in terms of health insurance coverage and access. Proponents of the Affordable Care Act (ACA) hoped that law’s major insurance coverage expansions and reforms would begin to bridge those gaps.
Evidence suggests that uninsured rates have declined among blacks and Hispanics under the ACA,1 but have these coverage gains reduced disparities between whites and ethnic and racial minorities? This brief seeks to answer that question and to examine if disparities in access to coverage and care are different in states that expanded Medicaid and states that did not.
We compared national averages between 2013 and 2015 for white, black, and Hispanic adults on three key measures of health care access to determine the effect of the ACA’s major coverage expansions on disparities:
- the share of uninsured working-age adults ages 19 to 64
- the share of adults age 18 and older who went without care because of costs in the past year
- the share of adults age 18 and older without a usual source of care. READ FULL ARTICLE
Preventive Health Care – What’s the Problem?
What’s the Problem?
CDC.gov I September 15, 2017
Nationally, Americans use preventive services at about half the recommended rate. Cost-sharing such as deductibles, co-insurance, or copayments also reduce the likelihood that preventive services will be used. One study found that the rate of women getting a mammogram went up as much as 9% when cost-sharing was removed.
Chronic diseases, such as heart disease, cancer, and diabetes, are responsible for 7 of every 10 deaths among Americans each year and account for 75% of the nation’s health spending. These chronic diseases can be largely preventable through close partnership with your healthcare team or can be detected through appropriate screenings when treatment works best.
Eating healthy, exercising regularly, avoiding tobacco, and receiving preventive services such as cancer screenings, preventive visits and vaccinations are just a few examples of ways people can stay healthy. The right preventive care at every stage of life helps all Americans stay healthy, avoid or delay the onset of disease, keep diseases they already have from becoming worse or debilitating, lead productive lives, and reduce costs.
And yet, despite the benefits of many preventive health services, too many Americans go without needed preventive care, often because of financial barriers. Even families with insurance may be deterred by copayments and deductibles from getting cancer screenings, immunizations for their children and themselves, and well-baby check-ups that they need to keep their families healthy. READ FULL ARTICLE
Why Every Health Care Organization Needs a Data Science Strategy
NEJM Catalyst I March 22, 2017
Harnessing the full potential of data requires developing an organization-wide data science strategy. Such strategies are now commonplace in most industries such as banking and retail. Banks can offer their customers targeted needs-based services and improved fraud protection because they collect and analyze transactional data. Retailers such as Amazon routinely collect data on shopping habits and preferences to profile their customers and use sophisticated predictive algorithms to tailor marketing strategies to customer demand.
Health care is a glaring exception. Individual pieces of data can have life-or-death importance, but many organizations fail to aggregate data effectively to gain insights into wider care processes. Without a data science strategy, healthcare organizations can’t draw on increasing volumes of data and medical knowledge in an organized, strategic way and individual clinicians can’t use that knowledge to improve the safety, quality, and efficiency of the care they provide.
A comprehensive data science strategy needs to address the quality of the underlying data, effective ways to analyze the data and a framework for keeping it secure. If an organization tries to aggregate and analyze poor-quality data, it may derive useless or even dangerous conclusions. An inadequate security framework may lead to unauthorized access and undermine the trust of patients and providers.
A carefully developed data science strategy will help achieve both precision medicine (helping to tailor treatments to patients) and the creation of learning health systems (helping to predict outcomes and identifying specific areas for improvement). Ideally, every decision a provider makes about a patient should be informed by the data of both that specific patient and other similar patients. In a learning health system, prior experiences improve future choices. Read Full Article